LEFT ATRIOVENTRICULAR VALVE
In-Depth AR Atlas Available
Read the comprehensive anatomy description with AR illustrations and videos
Read AR Atlas →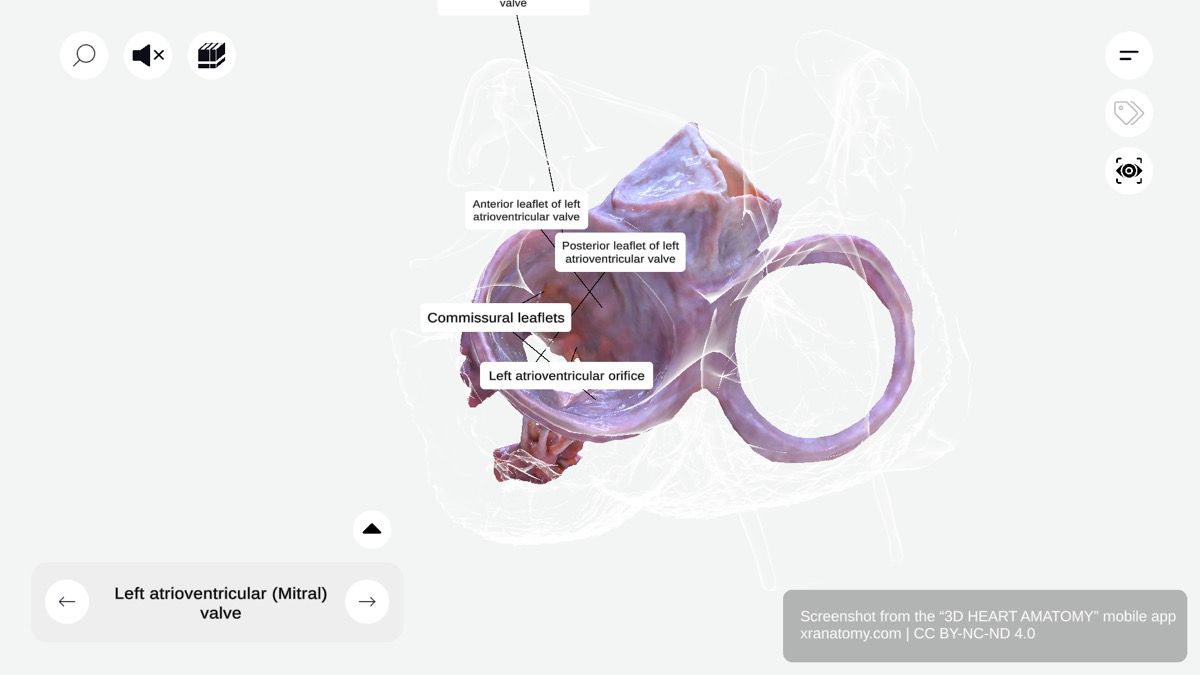
Left Atrioventricular Valve - Overview, Preview from the app.
WHY THIS MATTERS
The left atrioventricular valve (mitral valve) controls the flow of oxygen-rich blood from your left atrium into your left ventricle. Its leaflets, orifice, and tension apparatus work together to prevent backflow during ventricular contraction, keeping blood moving efficiently through your heart.
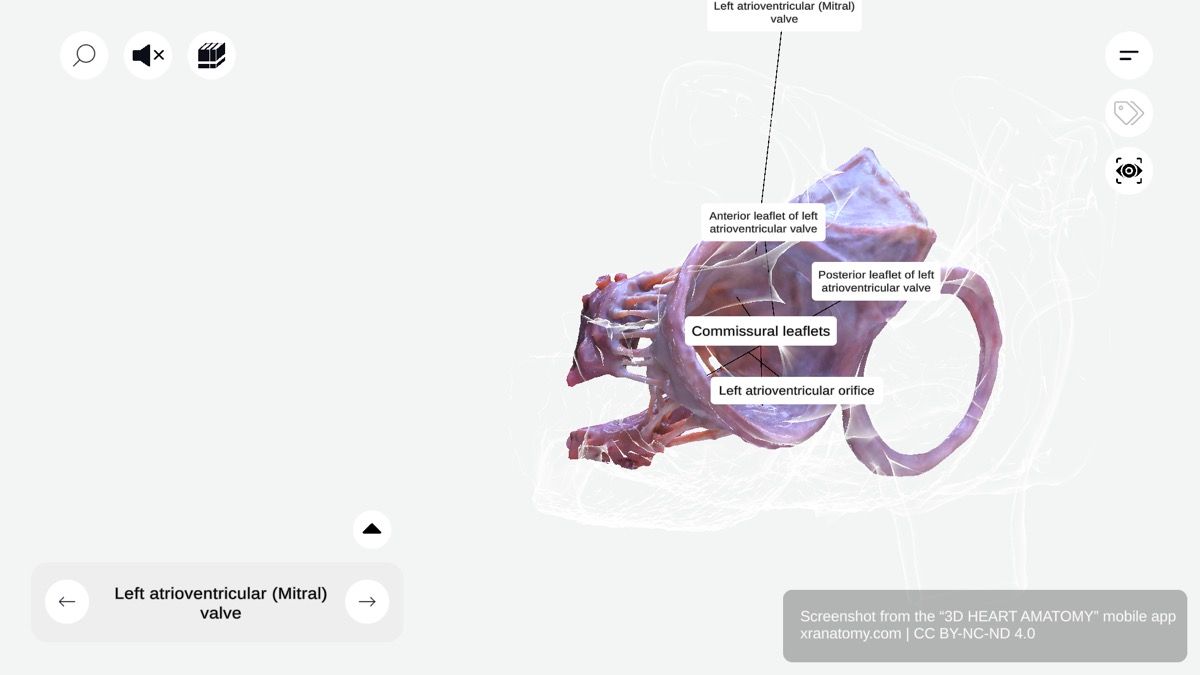
LEFT ATRIOVENTRICULAR VALVE
The left atrioventricular valve, also known as the mitral valve, regulates blood flow between your left atrium and left ventricle. It ensures oxygen-rich blood moves efficiently into your left ventricle and prevents backflow during ventricular contraction.
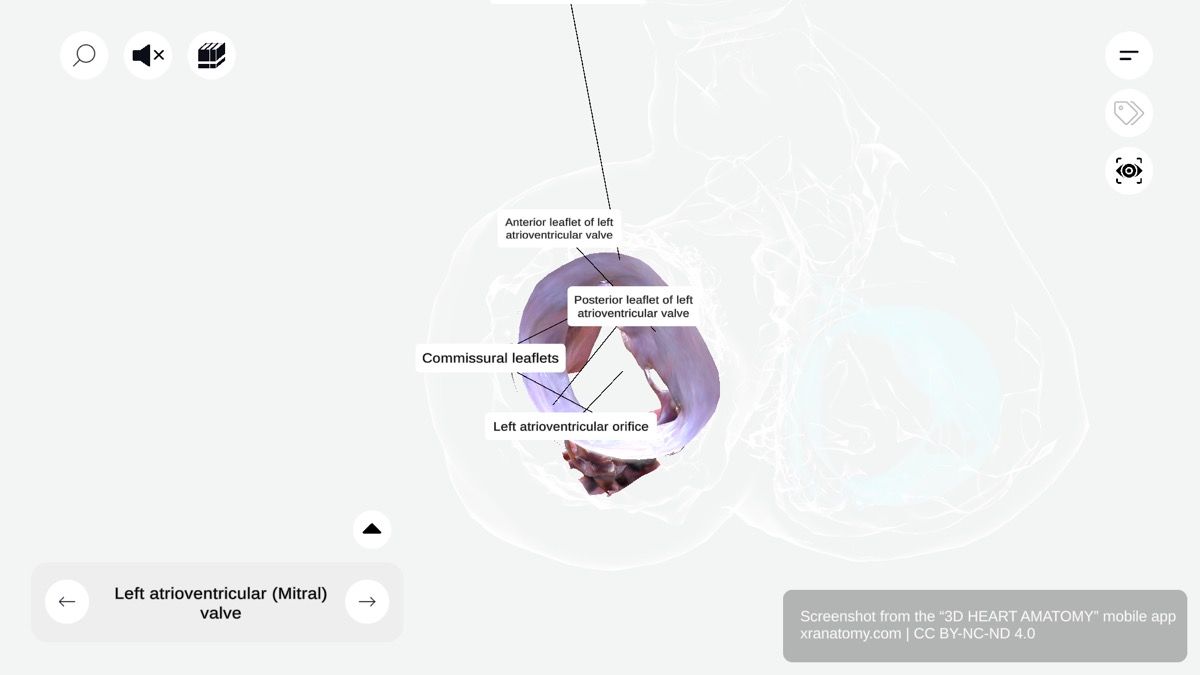
LEFT ATRIOVENTRICULAR ORIFICE
Left Atrioventricular Orifice, Preview from the app.
The left atrioventricular orifice is the opening between your left atrium and left ventricle. The mitral valve surrounds it and facilitates unidirectional blood flow through your heart.
LEAFLETS OF MITRAL VALVE
Mitral Valve Leaflets, Preview from the app.
The mitral valve is characterized by two main leaflets: the anterior leaflet (larger, adjacent to the aortic valve) and the posterior leaflet (smaller). Where these leaflets meet, commissural leaflets seal the orifice during ventricular contraction.
Anterior Leaflet
The anterior leaflet is the larger of the two leaflets and sits adjacent to the aortic valve. Its surgical subdivisions include the A1, A2, and A3 sections, which allow precise surgical identification.
Posterior Leaflet
The posterior leaflet is the smaller leaflet. Its surgical scallops include the P1, P2, and P3 scallops. These divisions aid surgical descriptions and interventions.
Commissural Leaflets
The commissural leaflets are smaller leaflets located at the convergence points where the anterior and posterior leaflets meet. They sit at the angles of the valve and are essential for sealing the orifice during ventricular contraction.
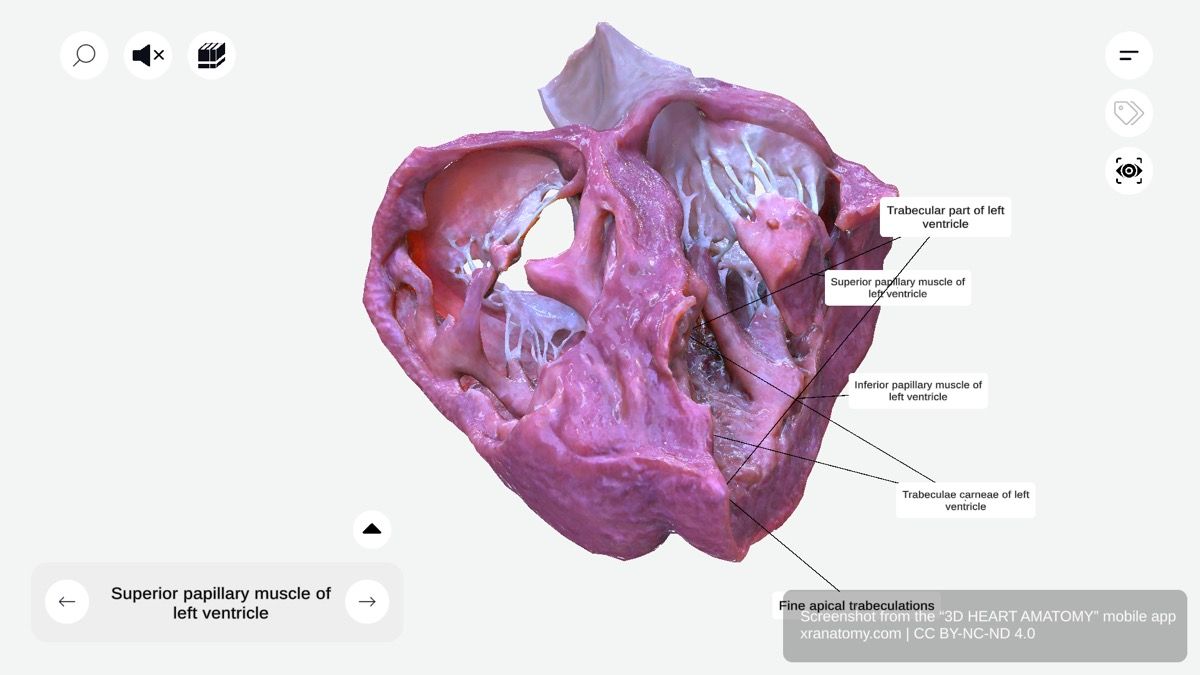
TENSION APPARATUS
The tension apparatus is essential for proper valve function. It prevents leaflet inversion into your atrium and prevents valve prolapse during ventricular systole. Its two components are the papillary muscles and the chordae tendineae.
Papillary Muscles
The papillary muscles contract with your ventricular myocardium. This simultaneous contraction with your ventricle allows them to tighten the chordae tendineae and secure your leaflets in position.
Chordae Tendineae
The chordae tendineae are tendinous cords that connect your leaflets to the papillary muscles. They are tightened during ventricular contraction and anchor the leaflets to prevent eversion.
Coordinated Action
The coordinated action of the tension apparatus ensures efficient valve closure in your heart and prevents regurgitation of blood into your left atrium.
CHECK YOUR UNDERSTANDING
1. What are the two main leaflets of the mitral valve, and which one is larger?
Reveal Answer
The anterior leaflet and the posterior leaflet. The anterior leaflet is the larger of the two and sits adjacent to the aortic valve.
2. What two components make up the tension apparatus?
Reveal Answer
The papillary muscles and the chordae tendineae. The papillary muscles contract with the ventricular myocardium to tighten the chordae tendineae, which anchor the leaflets in position.
3. What are the surgical subdivisions of the anterior and posterior leaflets?
Reveal Answer
The anterior leaflet has A1, A2, and A3 sections. The posterior leaflet has P1, P2, and P3 scallops. These subdivisions allow precise surgical identification.
WHAT'S NEXT
Next, you will explore the Root of Aorta. You will study the initial segment of the aorta emerging from the left ventricle, including the aortic valve, its leaflets, the sinuses of Valsalva, interleaflet triangles, and the supravalvular ridge.
Review this page again in 3 days to reinforce what you have learned.
BIBLIOGRAPHY
1. Gray H, Lewis W. Angiology. In: Anatomy of the Human Body. 1918. p. 526–542.
2. Gosling JA, Harris PF, Humpherson JR, Whitmore I, Willan PLT. Human anatomy: color atlas and textbook. 6th ed. 2017. 45–58 p.
3. Anderson RH, Spicer DE, Hlavacek AM, Cook AC, Backer CL. (2013). Anatomy of the cardiac chambers. In Wilcox’s Surgical Anatomy of the Heart (4th ed., pp. 13–50). Cambridge University Press.
4. Fritsch H, Kuehnel W. Color Atlas of Human Anatomy. Vol. Volume 2, Color Atlas and Textbook of Human Anatomy. 2005. 10–42 p.
5. Moore K, Dalley A, Agur A. Clinically Oriented Anatomy. Vol. 7ed, Clinically Oriented Anatomy. 2014. 132–151 p.
6. Ho SYen. Anatomy for Cardiac Electrophysiologists: A Practical Handbook. Cardiotext Pub; 2012. 5–27 p.
7. Standring S, editor. Gray's Anatomy: The Anatomical Basis of Clinical Practice. 41st ed. London: Elsevier; 2016.
8. Moore KL, Agur AMR, Dalley AF. Essential Clinical Anatomy. 5th ed. Philadelphia: Wolters Kluwer; 2015.