CALCANEUS ANATOMY
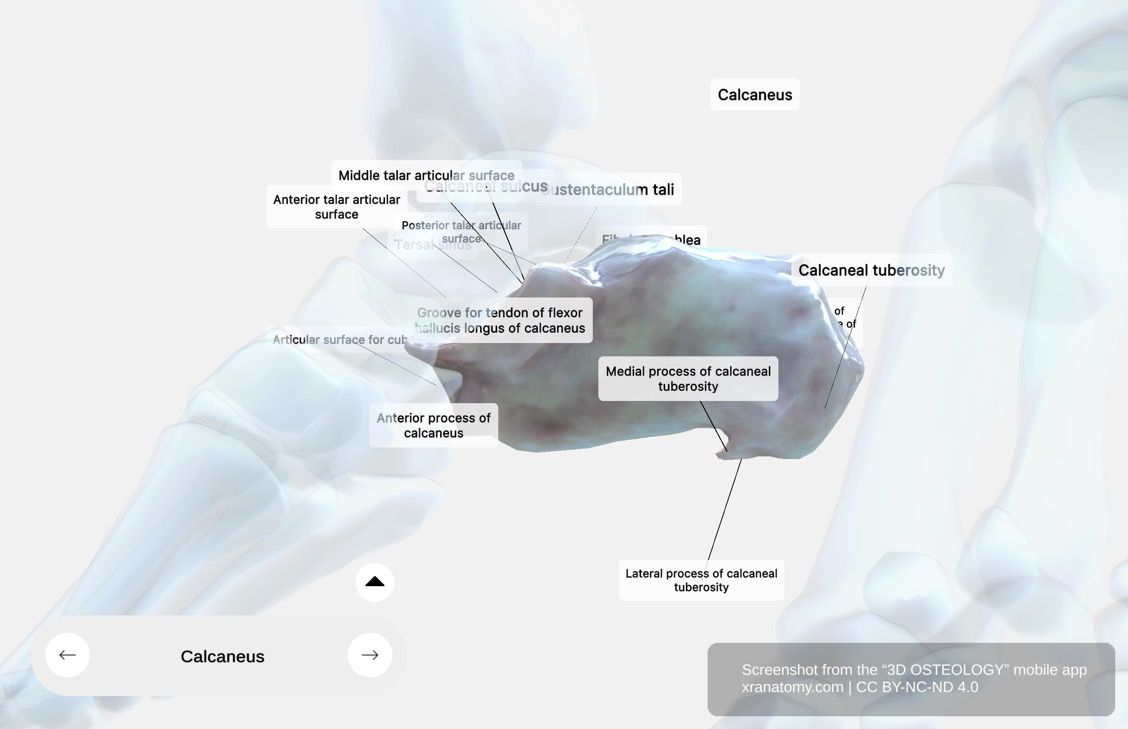
Calcaneus - X-Ray View, Preview from the app. Download 3D OSTEOLOGY for full 3D control—multiple views, x-ray mode, and unlimited zoom.
WHY THIS MATTERS
The calcaneus is the largest tarsal bone and forms your heel. It bears most of your body weight when you stand and acts as a lever for your calf muscles during movement. Understanding its tuberosity, sustentaculum tali, and articular surfaces helps you see how your foot transfers force from your leg to the ground.
GENERAL STRUCTURE
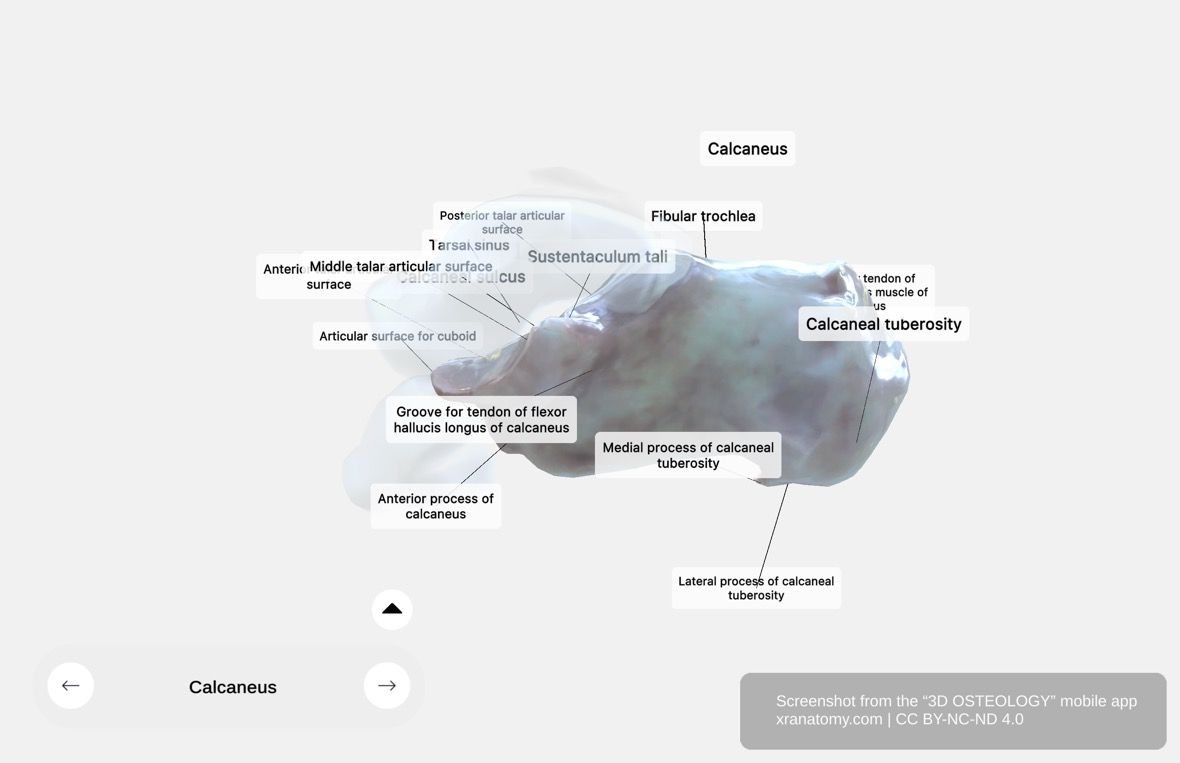
Calcaneus - General Structure, Preview from the app. Download 3D OSTEOLOGY for full 3D control—multiple views, x-ray mode, and unlimited zoom.
The calcaneus is the largest tarsal bone, located at the lower and posterior part of your foot. It plays a crucial role in transmitting your body's weight to the ground and serves as a lever for your calf muscles, contributing to movement and stability.
Role and Articulations
The calcaneus forms the heel of your foot and supports the talus above. Anteriorly, it articulates with the cuboid bone. This arrangement makes the calcaneus essential for weight-bearing and locomotion.
POSTERIOR EXTREMITY (CALCANEAL TUBEROSITY)
The posterior extremity of the calcaneus, also known as the calcaneal tuberosity, is the prominent projection that forms your heel. It is convex and wider below than above, divided into two processes: the medial process and the lateral process.
Medial Process
The medial process is the broader of the two processes. It serves as the attachment site for the abductor hallucis at its prominent medial margin and for the plantar aponeurosis anteriorly. This process is important for arch support in your foot.
Lateral Process
The lateral process is smaller, prominent, and rounded. It serves as the origin site for part of the abductor digiti minimi and contributes to your heel stability.
SUSTENTACULUM TALI
The sustentaculum tali is a shelf-like projection located above the concavity on the medial surface of the calcaneus. It is a critical structure for supporting the talus. A groove on its plantar surface accommodates the tendon of the flexor hallucis longus. The sustentaculum tali is important for subtalar joint stability.
TARSAL SINUS & CALCANEAL SULCUS
This region features two related landmarks: the calcaneal sulcus, a groove on the calcaneus, and the tarsal sinus, a tunnel formed when that groove meets the sulcus tali of the talus.
Calcaneal Sulcus
The calcaneal sulcus is a groove on the calcaneus located between articular surfaces. Together with the sulcus tali of the talus, it forms the tarsal sinus.
Tarsal Sinus
The tarsal sinus is formed by the sulcus calcanei of the calcaneus and the sulcus tali of the talus. It creates a tunnel filled with ligaments, including the interosseous talocalcaneal ligament. The tarsal sinus is important for subtalar joint stability.
TALAR ARTICULAR SURFACES
The calcaneus has three articular surfaces for articulation with the talus, forming the subtalar joint complex: the anterior talar articular surface, the middle talar articular surface, and the posterior talar articular surface.
Anterior Talar Articular Surface
The anterior talar articular surface sits on the calcaneus and articulates with the head of the talus. It is the smallest of the three surfaces.
Middle Talar Articular Surface
The middle talar articular surface sits on the sustentaculum tali and supports the talus. It is often continuous with the anterior surface.
Posterior Talar Articular Surface
The posterior talar articular surface is a large, oval-shaped facet on the dorsal surface of the calcaneus. It articulates with the talus and is the largest of the three surfaces.
ANTERIOR FEATURES
The anterior end of the calcaneus features three key landmarks: the fibular trochlea, which separates peroneal tendons; the articular surface for the cuboid, which forms the calcaneocuboid joint; and the anterior process, which projects forwards.
Fibular Trochlea
The fibular trochlea is often indistinctly marked. It acts as a bony pulley, separating the tendons of the fibularis longus (below) and fibularis brevis (above) muscles.
Articular Surface for the Cuboid
This articular surface has a triangular shape. It is concave from above downwards and lateralwards, and convex in the perpendicular direction. It forms the calcaneocuboid joint.
Anterior Process of the Calcaneus
The anterior process supports the articular surface for the cuboid and projects forwards. It forms part of the calcaneocuboid joint and is a common site for avulsion fractures.
CHECK YOUR UNDERSTANDING
1. What structure on the medial surface of the calcaneus supports the talus and has a groove for the flexor hallucis longus tendon?
Reveal Answer
The sustentaculum tali.
2. How many articular surfaces does the calcaneus have for the talus, and which is the largest?
Reveal Answer
Three articular surfaces. The posterior talar articular surface is the largest.
3. What two grooves combine to form the tarsal sinus?
Reveal Answer
The sulcus calcanei of the calcaneus and the sulcus tali of the talus.
WHAT'S NEXT
Next, explore the Cuboid Bone, the cube-shaped tarsal bone on the lateral side of your foot. You will study its peroneal sulcus, tuberosity, calcaneal process, and the articular surfaces it shares with the calcaneus and metatarsals.
Review this page again in 3 days to reinforce what you have learned.
BIBLIOGRAPHY
1. Henry G, Warren HL. Osteology. In: Anatomy of the Human Body. 20th ed. Philadelphia: Lea & Febiger; 1918. p. 129–97.
2. Standring S, editor. Gray's Anatomy: The Anatomical Basis of Clinical Practice. 41st ed. London: Elsevier; 2016.
3. Moore KL, Agur AMR, Dalley AF. Essential Clinical Anatomy. 5th ed. Philadelphia: Wolters Kluwer; 2015.